
The recent RECOVERY trial (Randomised Evaluation of COVid-19 thERapY) press release widely reported in the mainstream media claims that dexamethasone - a drug familiar to mountaineers for its treatment of high altitude illness - reduces death by up to one third in ventilated patients with severe respiratory complications of COVID-19. Prior to this 'major breakthrough', some physicians - and climbers in our forums - were pondering the similarities between the breathing difficulties and persistent cough commonly displayed by COVID-19 patients and the symptoms experienced by HAPE (High Altitude Pulmonary Edema) sufferers on high peaks.
'It's these symptoms that led to some making a link - shortness of breath, coughing, fatigue - but that's where the similarities end,' explains Jeremy Windsor, a Consultant in Anaesthetics and Critical Care at Chesterfield Royal Hospital and Senior Clinical Lecturer at the University of Sheffield. 'Despite what might have been published there's very little link between the two conditions.' Jeremy is also a seasoned mountaineer with ascents of Cho Oyu and Everest under his belt. In his mountain medicine blog, Jeremy underlined the key differences between the two conditions:
'HAPE is triggered by an irregular pattern of hypoxic pulmonary vasoconstriction that leads to widespread breakdown of the alveolar capillary membrane and the flooding of airways with fluid and cells, whilst Sars-Cov-2 infection causes destruction of the endothelial lining of small airways and swelling of neighbouring connective tissue.'
In layman's terms, the symptoms of HAPE are caused by fluid leaking across the thin barrier between the lungs and blood vessels, whereas the effects of COVID-19 are due to widespread damage and swelling to the lining of the airways.
A similarity in symptoms, therefore, does not mean that the pathological processes of the two diseases are the same. 'COVID-19 Lung Injury is Not High Altitude Pulmonary Edema', the title of a paper in High Altitude Medicine & Biology Vol. 21, No. 2, reads.
In the RECOVERY trial, a total of 2104 patients were randomised to receive dexamethasone 6-8 mgs once a day (either by mouth or by intravenous injection) for ten days and were compared with 4321 patients randomised to usual care alone. Among the patients who received usual care alone, 28-day mortality was highest in those who required ventilation (41%), intermediate in those patients who required oxygen only (25%), and lowest among those who did not require any respiratory intervention (13%). Dexamethasone reduced deaths by one-third in ventilated patients and by one fifth in other patients receiving oxygen only. There was no benefit among those patients who did not require respiratory support. Based on these results, 1 death would be prevented by treatment of around 8 ventilated patients or around 25 patients requiring oxygen alone.
Over the past five months, Jeremy has been on the front lines of COVID-19 as a critical care physician. Chesterfield Royal is a district general hospital with a catchment area of approximately 400,000, where nearly 300 patients have died from the disease. 'We normally run a 15 bedded critical care unit,' Jeremy says. 'During the busiest times of the COVID epidemic we expanded to accommodate around 30 patients, the majority of which had COVID.' The hospital focused primarily on COVID-19 and halted non-emergency admissions for almost every other illness. 'Only emergencies were admitted and treated,' he adds. 'Everything else was out on hold.' The Chesterfield Royal enrolled one of the largest groups of patients for the RECOVERY study, approximately 150.
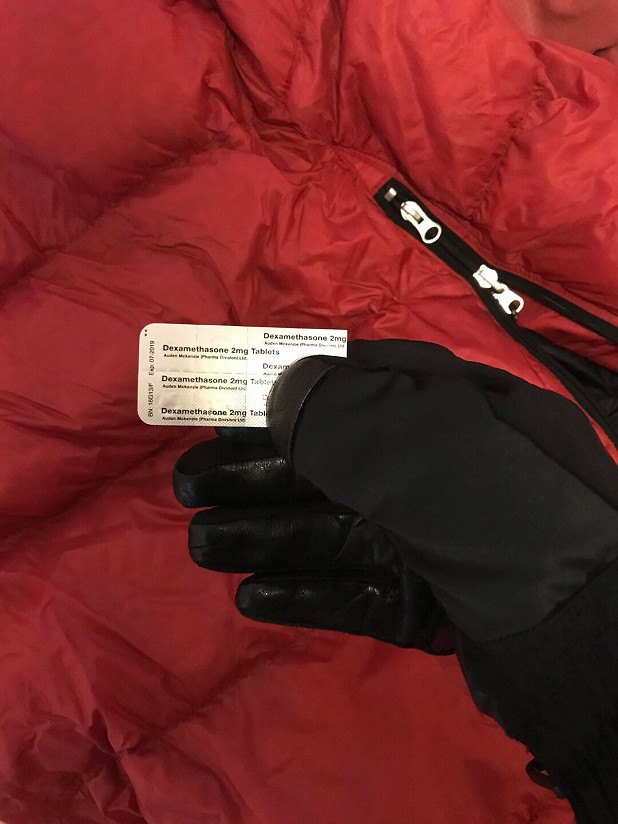
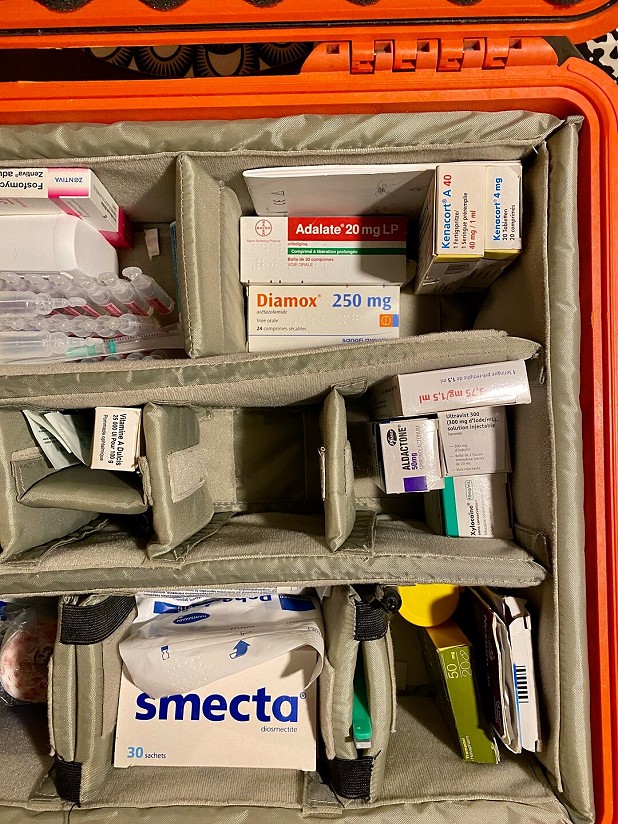
Dexamethasone is predominantly used for HACE (High Altitude Cerebral Edema) to reduce brain swelling. 'It can buy precious time and allow victims to be evacuated. Sometimes it's successful enough to get a HACE victim moving independently, which can be a god send high on a mountain,' Jeremy explains. 'It's sometimes used to treat HAPE - especially if there's any suspicion of HACE, as both conditions can often occur together.'
As a preventative drug on high altitude expeditions, opinions on its effectiveness remain mixed. 'There is some research that points to its use in preventing HAPE and AMS (Acute Mountain Sickness), however most who practise in mountain medicine strongly believe that it doesn't help the acclimatisation process but instead masks the symptoms of AMS and HAPE,' Jeremy explains. 'Stop taking it at altitude and these conditions can develop very quickly.' Dexamethasone's initial purpose as a first aid, emergency medicine has morphed into one of performance enhancement for those looking for a quick-fix for ascents of Everest and elsewhere, alongside EPO, Diamox and of course - supplementary oxygen.
Being one of the cheapest available drugs globally, dexamethasone was one of many drugs being trialled in countries such as Italy, who treated cases before the UK and most of the world. Dexamethasone doesn't target the virus specifically, but rather enables the patient's lungs to keep functioning and therefore assist the body in fighting the virus.
The use of a steroid to promote recovery in a viral disease that relies heavily on a strong immune system might seem counterintuitive, since steroids are immunosuppressive. 'That's always a real concern with steroids - too much and there's a real risk of the body not being able to fight an infection,' Jeremy explains. 'Over the years it's become clear that our understanding of how steroids work is limited. There's much we don't know. For a start, how do steroids work in COVID but not in other viral chest infections such as SARS or MERS?'
Steroids are nonetheless commonly used to treat a number of conditions, but in small doses. 'In chest complaints, it's probably best known in asthma and flare ups of chronic obstructive pulmonary disease (COPD),' Jeremy says. Side effects of long-term use of steroids can be extremely serious. In 2009, a young American mountaineer's Everest expedition was cut short when he suffered internal bleeding due to the damage caused to his stomach lining by dexamethasone. The young man's doctor had prescribed him a long course of the drug to assist acclimatisation and in addition to the bleeding, his dependence on it meant that his body could no longer produce its own natural steroids.
Despite the media buzz, the RECOVERY paper hasn't been peer reviewed and published yet. 'I think that the 10 day course of 6-8mg given in the RECOVERY trial was unlikely to cause significant side effects, but without the publishing of the RECOVERY trial its impossible to say,' Jeremy explains. He is aware of the trial's limitations and bias, having selected participants and had the option to withdraw patients if the drug appeared to be worsening their state.
'The lack of review is highly unusual, but these are unusual times. Nevertheless, rigorous peer review is vital,' Jeremy says. 'Already, a paper published in The Lancet has been withdrawn. Authors are under pressure to publicise their work, journals want to be the first to publish and governments want solutions. This generates enormous pressure and can lead to bad science. We really need to see the study after peer reviewers have pored over it - the methodology and data analysis especially - so that we know the conclusions are reliable.'
But even following the study's review, Jeremy maintains that he will still need convincing. 'I can't name a drug or technological intervention that has led to such an enormous reduction in critical care mortality,' he admits. 'Critical care is all about doing lots and lots of small things well. Think of the "marginal gains" that David Brailsford has described so well. I'm sceptical that one intervention, that hasn't a proven track record in treating viral pneumonia, should be this effective.'
Normally, new treatments are accepted by critical care physicians after a number of studies have been done. 'It's not unusual for a single study to show a brilliant result but then several more showing lesser improvements and in some cases worse outcomes,' Jeremy says. 'It's just the way science works and unfortunately we've not had the time to work through this process.'
UK Prime Minister Boris Johnson and the NHS announced immediate approval of the drug's use. 'This astounding breakthrough is testament to the incredible work being done by our scientists behind the scenes,' UK Health Secretary Matt Hancock told the press. Meanwhile, physicians across the country are faced with the decision as to administer dexamethasone or not.
'With all that said, mortality runs at around 50% in those who succumb so badly to COVID that they need admitting to critical care. Many of these are young people, often with young families, working in the NHS or other caring professions,' Jeremy explains. 'Would I prescribe dexamethasone given the information available? Yes, I trust the authors of the study and the scientific advisors supporting the study but I shouldn't have to. I should be able to see the study in its entirety and make my own decision. For now I can't.'
Faced with dying patients, Jeremy wrote in his blog, physicians want to "do something." But the answer is not to "do something", he summarised, but simply to "do no harm"- the guiding principle for medical professionals as outlined in the Hippcractic Oath. Until the RECOVERY trial has undergone peer review, dexamethasone might still give both patients and their physicians some time and room to breathe until a vaccine or specific treatment is developed.
Read Jeremy's mountain medicine blog.
More Articles






























































Comments
What a great article. I admit I was a bit sceptical before reading it due to the headline style title but that was brilliant. Enough detail from a expert for the interested layman without being overwhelming, a good synopsis of the research and a nice personal "Op Ed" style final two paragraphs.
Quality work UKC, well done.
So not fully proven but available, in use and it appears, saving lives. Every little helps in this current fight. Well worth the read.
Good article, well done UKC for such and informative and balanced report.
Very helpful article.
I'm glad the potential immunosuppressive effects of steroids are mentioned. I've read a few comments suggesting that it was obvious to use something like dexamethasone once the importance of the inflammation was realised, but using steroids in the presence of an active viral infection can run a real risk of making the infection worse. Of course, not all steroids are the same, but still, it's a slightly counter-intuitive thing to do.
This UKC article is great news but this one isn't I'm afraid.
https://www.theguardian.com/us-news/2020/jun/30/us-buys-up-world-stock-of-key-covid-19-drug
'Looking after your own?'